Welcome and greetings to every one who are visiting my blog. This is an online E log platform to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. I have been given this case in order to solve in an attempt to understand the topic of patient's clinical data analysis to develop my competency in reading and comprehending clinical data and come up with a diagnosis and treatment plan.
A 40year old female came to the opd with the chief complaints of abdominal distention and facial puffiness and itching since 1year, shortness of breath since 5days and pedal edema since 5days.
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 1 year back then she developed abdominal distension, facial puffiness,itching all over the body and 5 days ago she developed pedal edema and SOB grade 3.
she had an episode of vomiting two days back which contained food particles. It was relieved on medication.
HISTORY OF PAST ILLNESS:
she developed B/L Knee pain - since 3years, onset - insidious, gradually progressing, type- pricking, more at the night, aggravated on walking, relieved on sitting and sleeping, no radiation and is under medication(demisone 0.5 mg and acelogic SR)
She developed abdominal distension and facial puffiness one year back.
She also developed itching and skin lesions and was diagnosed as tinea and was given medications.
Not a K/C/O DM/HTN/ asthma / Ischemic heart disease / epilepsy / TB
FAMILY HISTORY:
No significant family history
PERSONAL HISTORY:
Patient is a daily wageworker but stopped it since 3months.
DIET MIXED
APPETITE decreased
SLEEP:normal
BOWEL AND BLADDER HABITS : decreased urine output
ADDICTIONS: No
GENERAL EXAMINATION:
Patient is concious coherent and coperative, well oriented to time palce and person
No pallor, cyanosis clubbing lymphadenopathy,icterus.
VITALS
BP 110/80
PR 90bpm
TEMP 98.5degrees F
SPO2 98 @ RA
GRBS 106
SYSTEMIC EXAMINATION
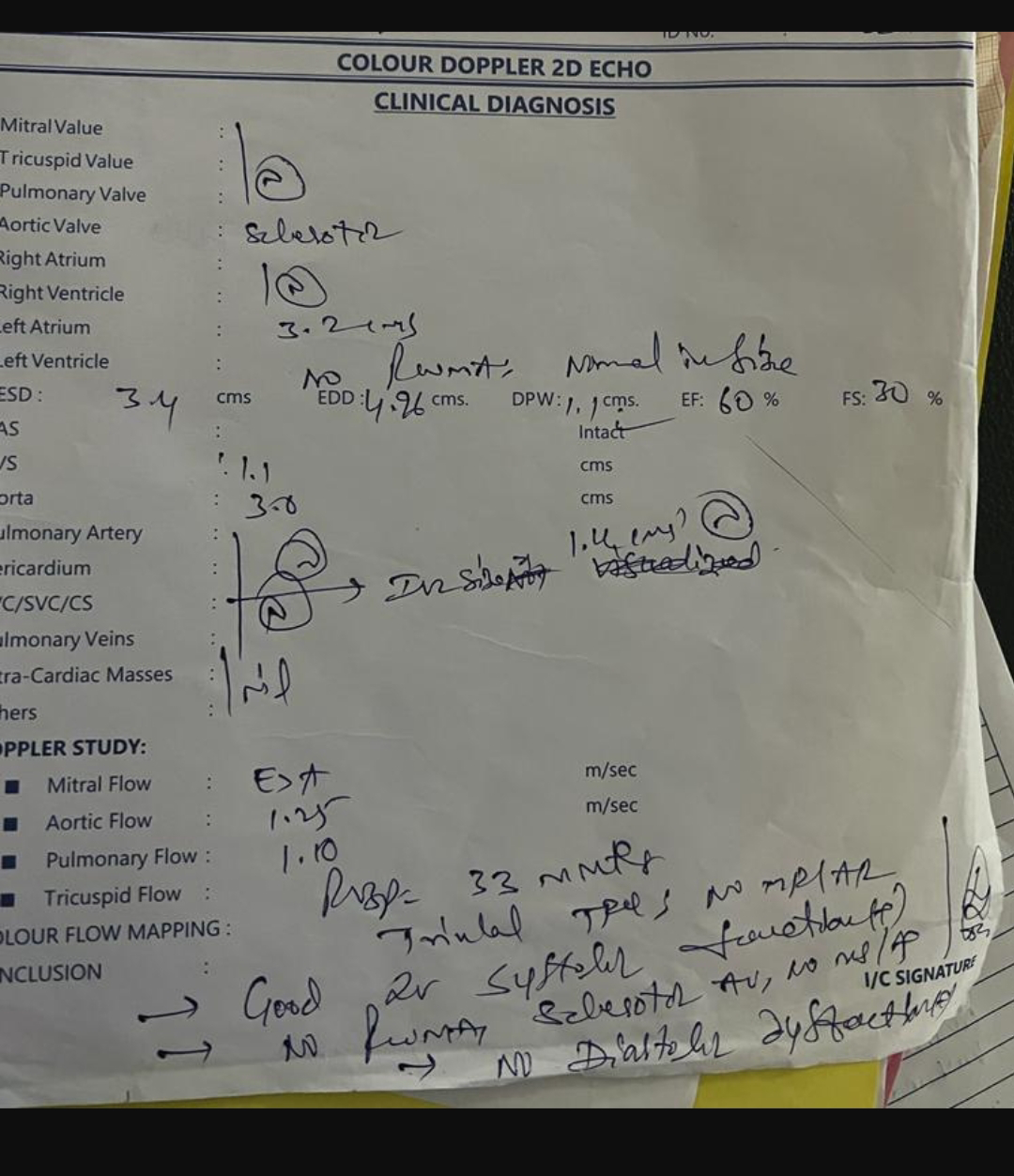
CVS:
S1&S2 Heard,no thrills,no murmurs
RESPIRATORY:
Vesicular breath,trachea in central position,no wheeze,no dyspnea.
ABDOMEN:
Distended, no tenderness ,no palpable masses,.normal hernial orifices,no bruit
Spleen,liver non palpable
CNS:
Concious
Speech:normal
Gait:normal












Comments
Post a Comment